Side Effects of Chemical Peels
A well-designed peel is a controlled medical act: expected skin responses (tightness, flaking, short-term redness) are not “complications.” True complications are uncommon and usually preventable with correct patient selection, chemistry control, and strict aftercare.
Key principle: side effects increase when treatment becomes too aggressive, when products are used incorrectly at home, or when post-peel rules (sun, alcohol-based cosmetics, occlusion) are ignored.
What is normal after a peel?
- Warmth / mild burning during application (should remain tolerable and monitored).
- Tightness and dryness during the first 48–72 hours.
- Flaking (desquamation) from day 2–5 (varies with peel type and skin condition).
- Mild redness that progressively decreases.
- Temporary sensitivity to wind, heat, friction, and active cosmetics.
These changes reflect controlled renewal of the stratum corneum and barrier recovery. In modern protocols, the goal is high safety + predictable recovery.
Warning signs: when to contact a clinician
Contact us promptly if you have:
- Redness that worsens after day 3–4 instead of improving
- Intense swelling, especially around eyes
- Oozing, crusting, increasing pain, or fever
- New blisters or “raw” areas
- Darkening patches that appear rapidly (suspected PIH)
Emergency (same day) if:
- Severe pain not relieved by cooling measures
- Rapidly spreading swelling or hives
- Signs of infection (pus, expanding redness, systemic symptoms)
- Eye exposure or visual symptoms
Most common side effects (and why they happen)
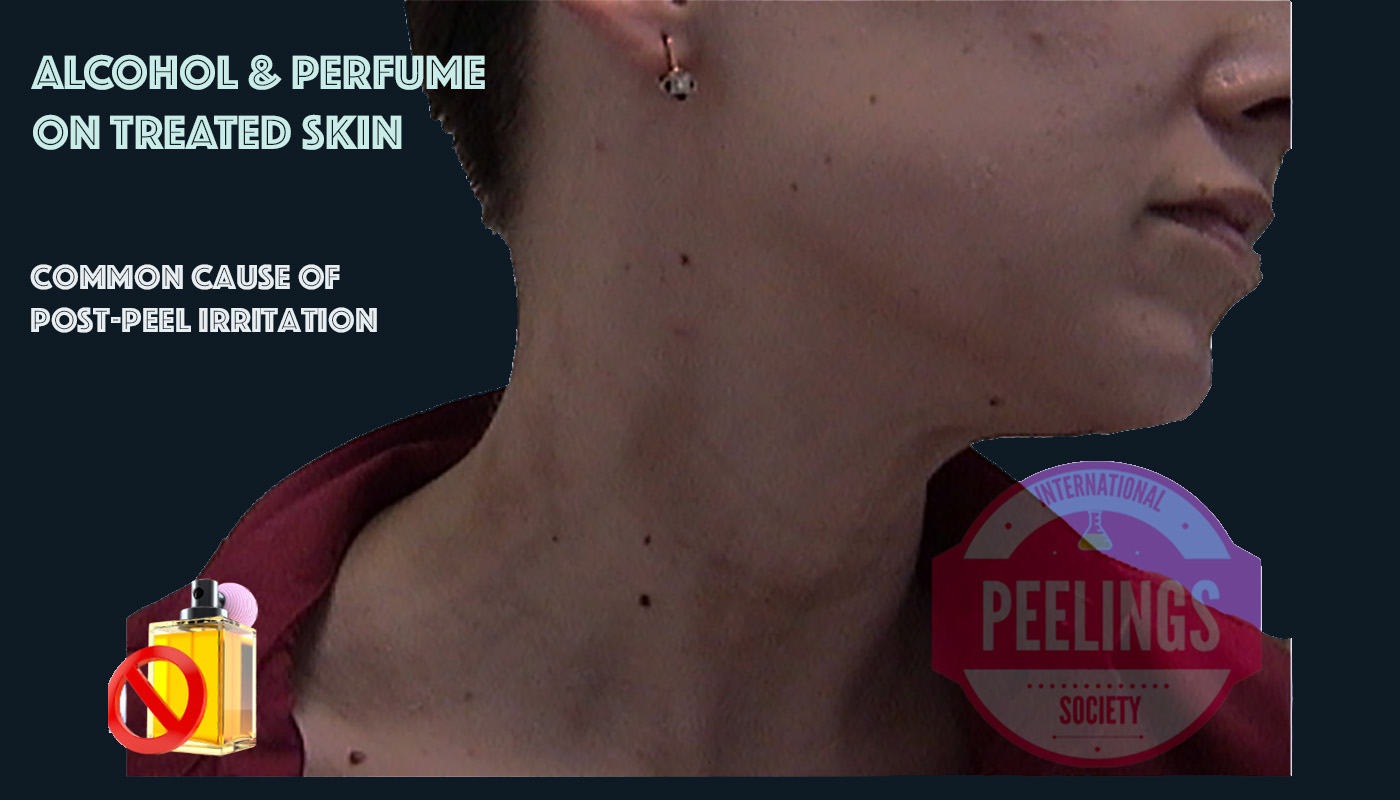
- Irritation / dermatitis: barrier weakened + friction, heat, or alcohol-based products.
- Acne flare / comedones: occlusion and comedogenic cosmetics used during healing.
- Post-inflammatory hyperpigmentation (PIH): inflammation + UV exposure + wrong intensity for phototype.
- Prolonged redness: over-treatment, repeated aggressive sessions, or inadequate recovery time.
- Herpes reactivation (HSV): in predisposed patients if prophylaxis is omitted.
Why side effects happen (risk management)
Most complications are not “bad luck.” They are typically linked to: inadequate diagnosis (melasma vs PIH), insufficient skin preparation, poor chemistry control (pH/solvents), wrong peel intensity, or incorrect aftercare.

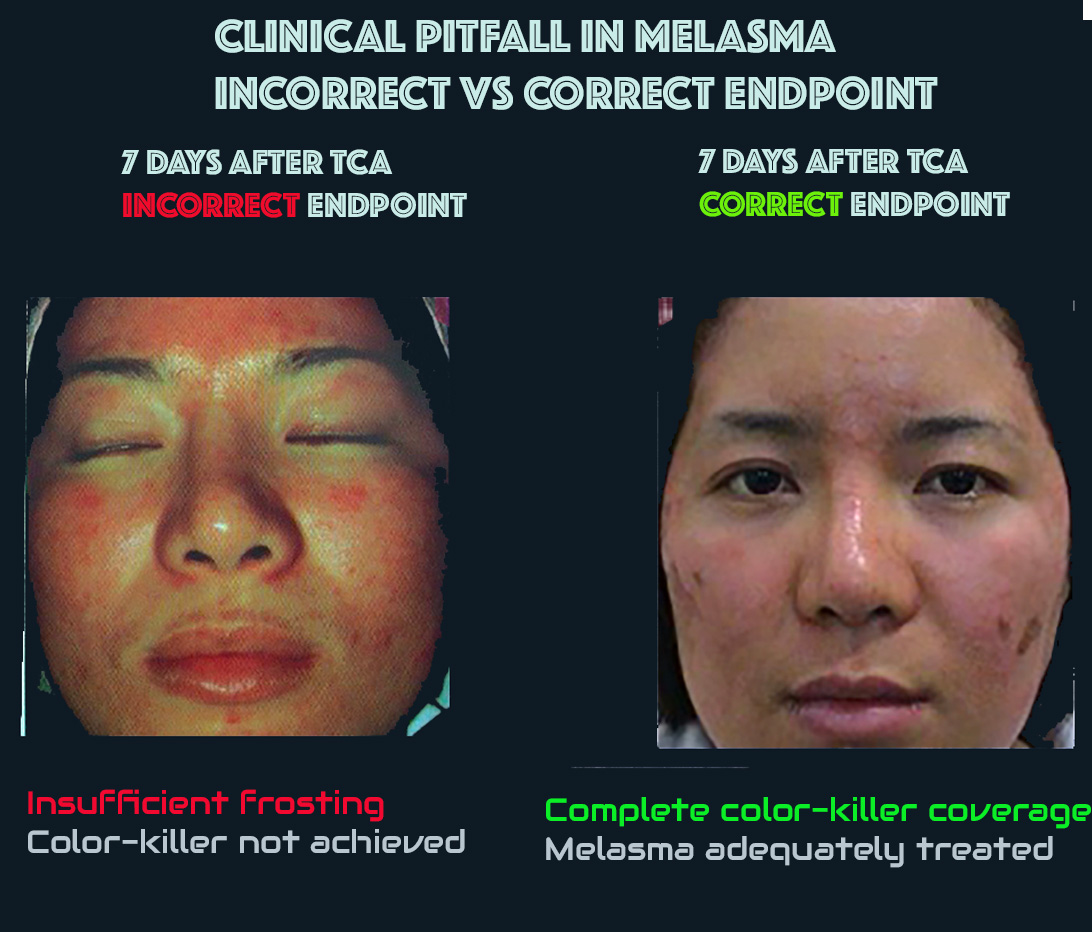
Clinical pitfall: “frosting” does not equal correct endpoint
In melasma, chasing an intense, uniform frosting can worsen inflammation and trigger PIH. Correct management prioritizes controlled sessions, photoprotection without alcohols, and pigment-safe strategies over aggressive endpoints.
Prevention: what reduces side effects the most
Before the peel
- Accurate diagnosis (melasma vs PIH vs post-acne marks)
- Phototype-based planning and realistic intensity
- Skin preparation when indicated (barrier + pigment control)
- HSV prophylaxis for patients with history of cold sores
After the peel
- Strict sun avoidance + broad photoprotection without Alcohols
- No friction, scrubs, waxing, or heat exposure
- Use only clinician-approved recovery products
- Avoid alcohol-based toners, perfumes, and “denatured alcohol” cosmetics

What to do if a reaction occurs
- Stop all active cosmetics (retinoids, acids, scrubs, “brightening” serums, fragrance).
- Cool compresses (short cycles) and barrier-only recovery care.
- Strict photoprotection without Alcohols and physical sun avoidance.
- If symptoms worsen: contact your clinician for assessment and tailored care.
Important: Do not “fix” a reaction by adding random products. Mixing acids, alcohol-based cosmetics, perfumes, or occlusives can amplify inflammation.
Downtime (“social eviction”): setting expectations is part of safety
Many negative experiences come from poor expectation management. A safe protocol includes: an explained recovery timeline, what is normal on day 1–3, and how many sessions are planned.

Clinical case library: complications that were corrected
The examples below illustrate a consistent principle: when a strategy is wrong (too aggressive, wrong indication, poor chemistry control), skin outcomes can deteriorate. With a safer, protocol-guided approach, many cases can be corrected over time.

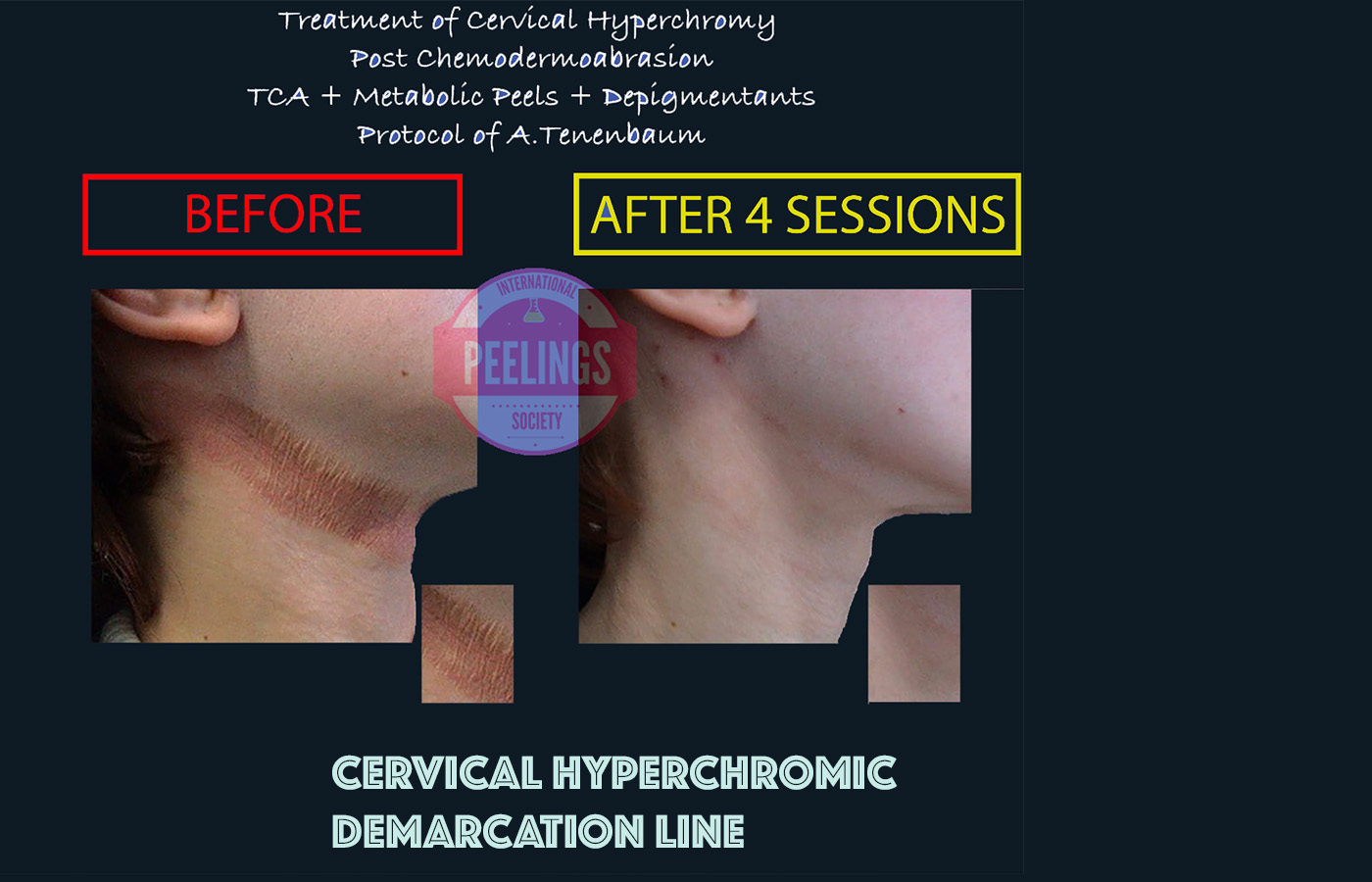
Progressive improvement after repeated TCA and metabolic peel sessions. Early sessions may appear worse; continuation of the protocol is essential for correction.
Take-home rules
- Prefer protocol-guided peels over “one-size-fits-all” marketing peels.
- Alcohol free Photoprotection is not optional—it is part of the treatment.
- Avoid perfume, alcohol-based toners, and random active cosmetics during healing.
- If pigmentation appears, do not intensify the peel—reduce inflammation first.
Need a safer plan?
If you experienced a reaction or want to reduce risk before starting a peel series, consider a clinician-guided approach. A correct diagnosis and recovery plan can make the difference.
Next steps
- Review contraindications
- Follow aftercare rules
- Use approved recovery products
