Protocol
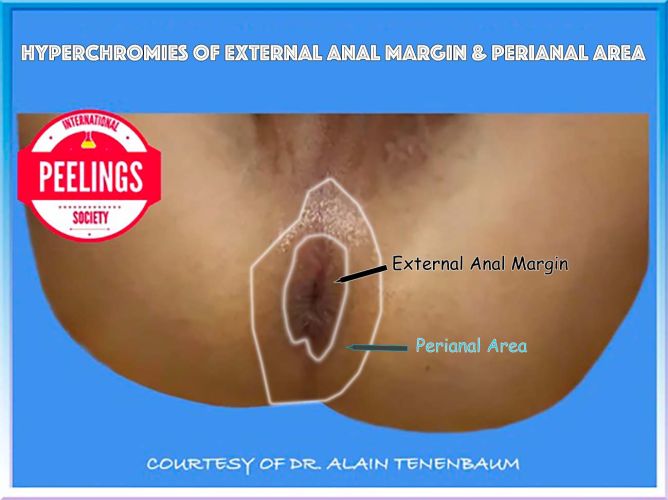
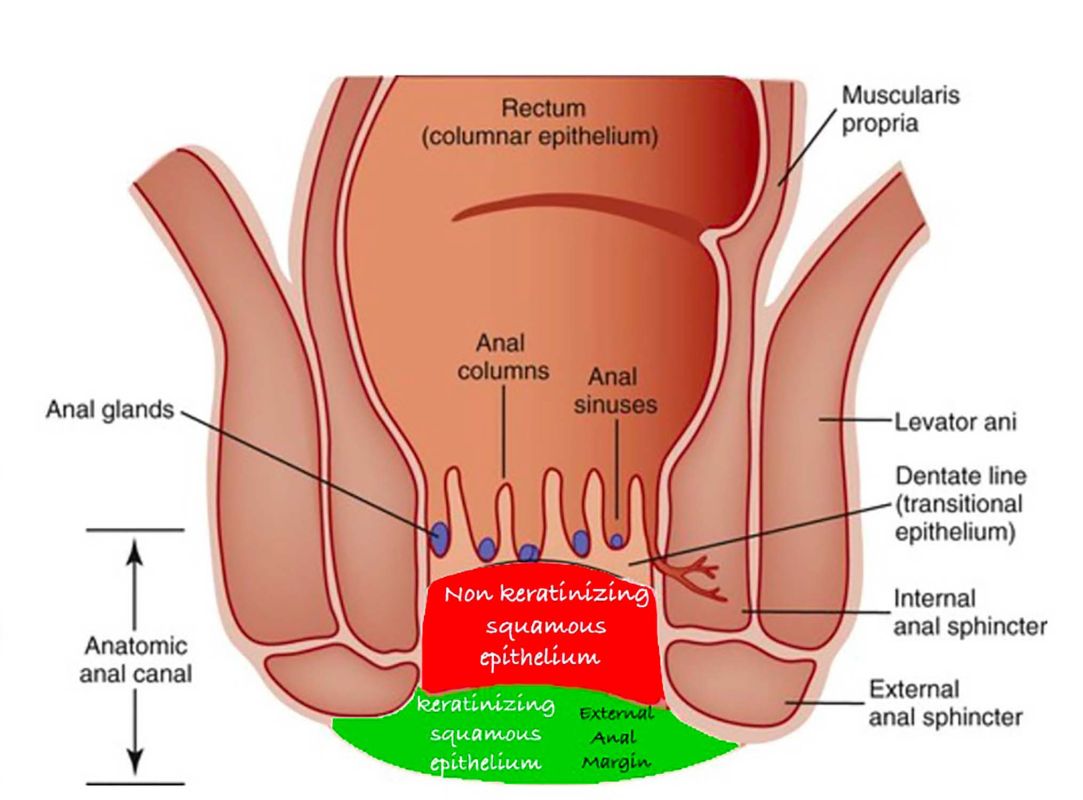
EXTERNAL ANAL MARGIN
&
PERIANAL AREA
EXTERNAL ANAL MARGIN
&
PERIANAL AREA
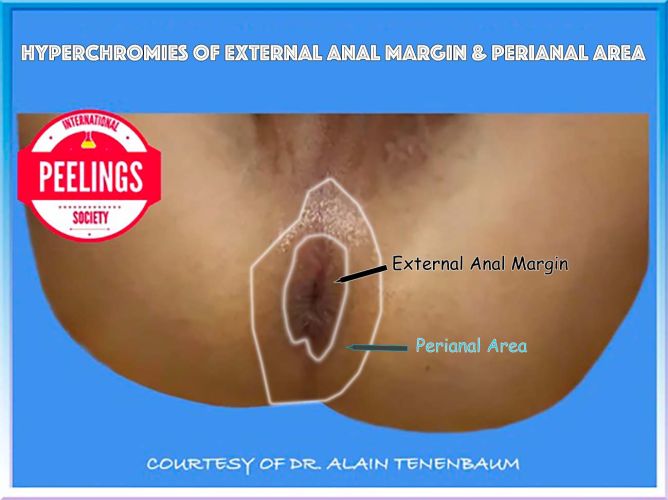

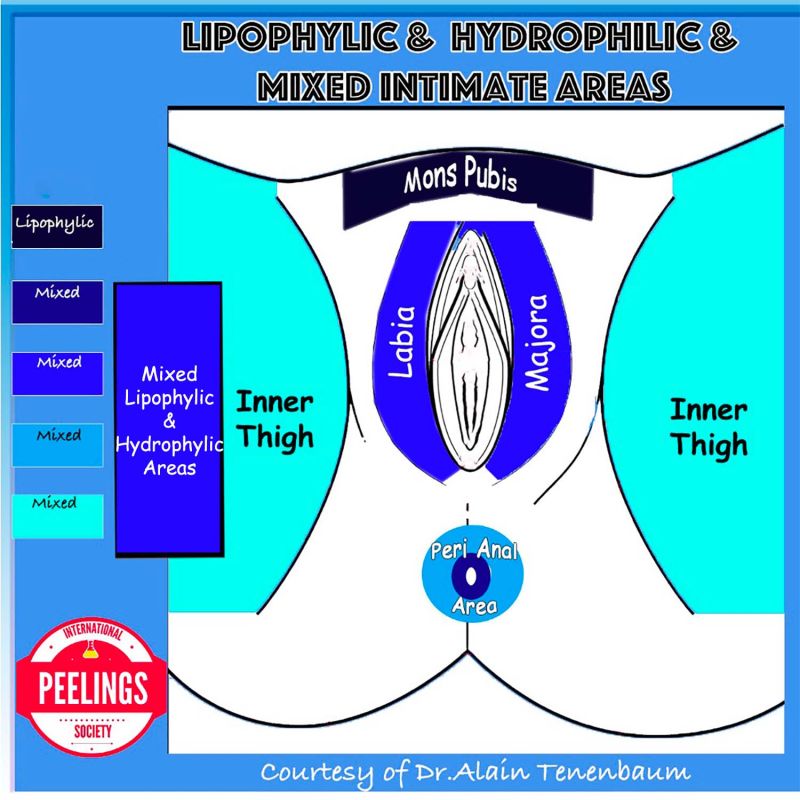
When selecting the appropriate acids as depigmenting agents (‘color killers’), 3 key parameters must be considered: whether the target area is hydrophilic or lipophilic, the relative thinness or thickness of the tissue, and the overall safety profile.
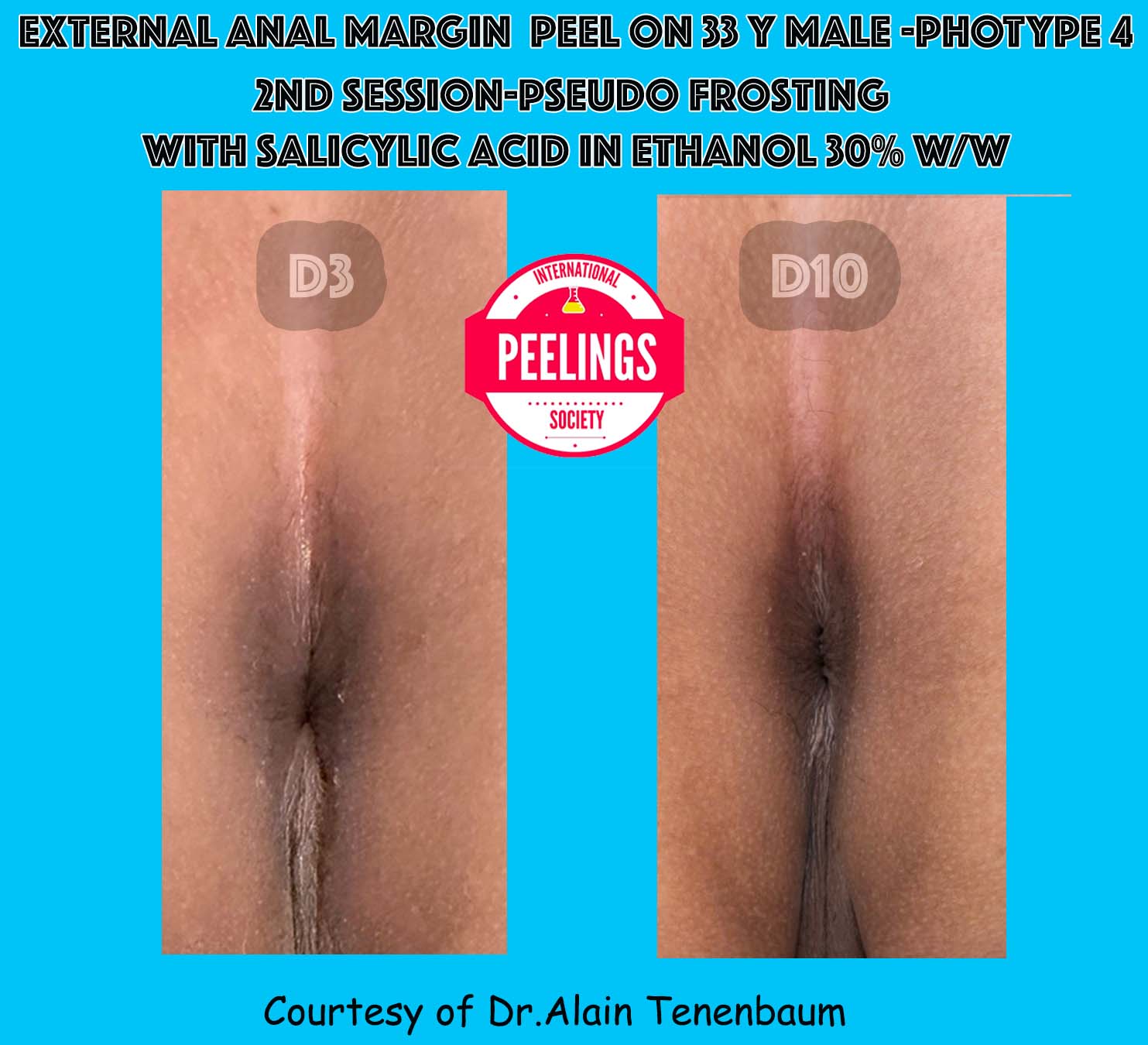
Lipophilic areas → respond best to salicylic acid (BHA).
Thick epidermis → use solution formulations (e.g., TCA, salicylic acid in ethanol) → faster penetration.
Thin epidermis → use gel/cream formulations, slower penetration, and at lower concentrations for safety.
hydrophilic vs. lipophilic (determine whether the target area retains water or oil )
avoid agents that could migrate beyond the target (e.g., do not use TCA on the external anal margin, as accidental spread into the rectum may cause injury)
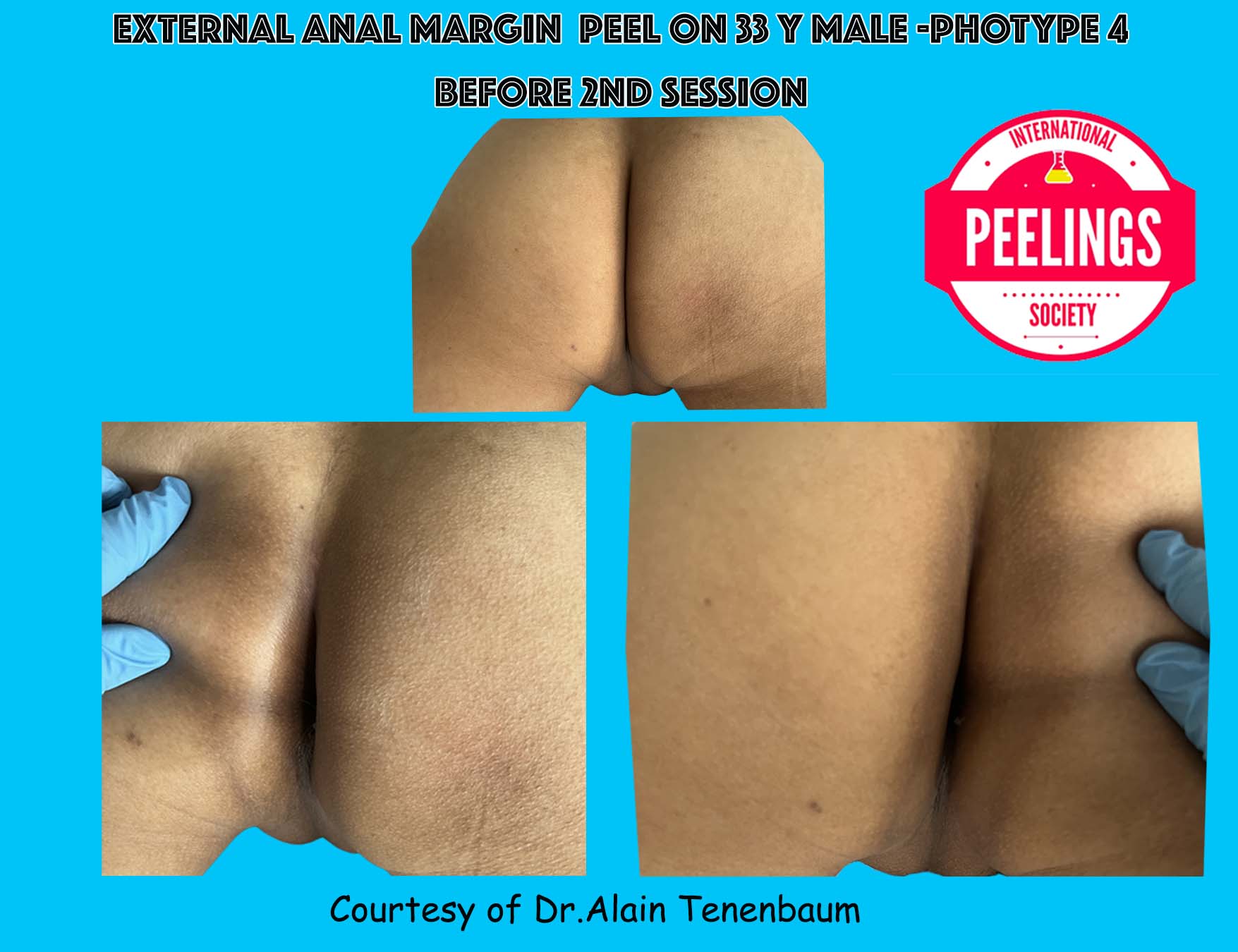
The external anal margin is generally thicker and drier compared to the rest of the perianal skin
This area has a tougher skin texture, which helps protect it from friction and abrasion
The external anal margin is generally thicker and drier compared to the rest of the perianal skin
This area has a tougher skin texture, which helps protect it from friction and abrasion

The perianal area is typically considered a dry area, as it has a low concentration of sebaceous (oil-producing) glands
However, it can become moist due to sweat, mucus, or hygiene-related factors
The skin in this area can be sensitive, so it's important to maintain proper hygiene without causing irritation
The perianal area is typically considered a dry area, as it has a low concentration of sebaceous (oil-producing) glands
However, it can become moist due to sweat, mucus, or hygiene-related factors
The skin in this area can be sensitive, so it's important to maintain proper hygiene without causing irritation

to get a frosting

Step 1 :Cleansing with ASEPTISKIN:
Begin with a thorough cleanse to remove any makeup, oils, and impurities from the skin.
This ensures that the peeling agents can penetrate effectively.
Use a gentle, non-exfoliating cleanser to avoid stripping the skin.

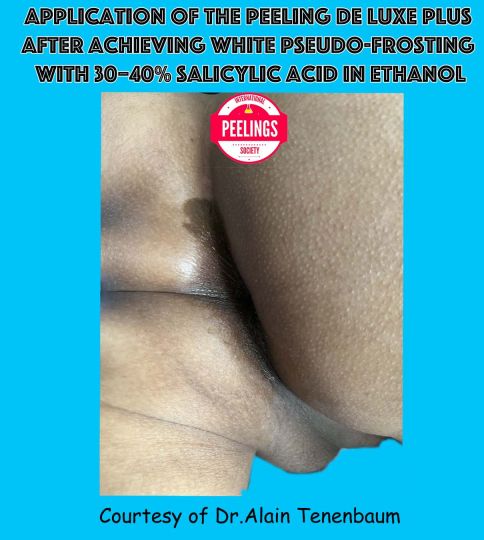
Step 2 :Applying the Color Killers Acids
Even low concentrations can trigger rebound (especially if TCA is buffered)
TCA for those indications is not first-line unless:
Combined with metabolic peels (e.g., Peeling de Luxe Plus) to control depth and inflammation
➡️ Recommendation:
Only apply as a colorkiller treatment, followed immediately by Peeling de Luxe Plus once the frosting covering the pigmented color is reached out.
Vehicle:
In ethanol → Better penetration, but higher irritation.
In glycerol → Safer, more controlled release
➡️ Recommendation: Salicylic acid in glycerol can be effective, especially when combined with melanin synthesis inhibitors (e.g. kojic acid, like StretchPeel ) before and after the peel.

Step 3 : Peeling de Luxe Plus (Frosting Stopper)
The following key points should be observed:
Frosting Appearance for the Lesion Area:
The frosting must appear white and should completely cover the lesion area.
To achieve this, a highly concentrated acid is required.
Do not use our frosting stopper on the Lesion Area during Frosting !
Wait the Defrosting to apply it on the Lesion Area .
Frosting Control for the Narrow Peri-Wound Area:
If the frosting turns white in the narrow peri-wound area adjacent to the lesion, it should be stopped using our frosting stopper.
This can be managed with a less concentrated acid, although it will still induce frosting.
No Frosting for the Larger Area Surrounding the peri-wound area:
For the larger surrounding area around the peri-wound, a low-concentration acid should be applied.
This concentration should be sufficient to avoid frosting in the area.
There is mostly no need to use the frosting stopper in the larger area surrounding the narrow peri wound area
Step 4 : Stretchpeel (Depigmentant Cream)
Apply it
- on The Lesion Area , above Peeling de Luxe Plus after defrosting
- Apply it to the narrow peri-wound area immediately after using Peeling de Plus, and again over it once the gray frosting appears.
Step 5 : Les Félins (Moisturizing Cream)
Apply it on the Larger Area Surrounding the peri-wound area.
Apply Les Félins non-greasy, fast-absorbing moisturizing cream to the untreated areas to ensure consistent hydration across both treated and untreated zones.

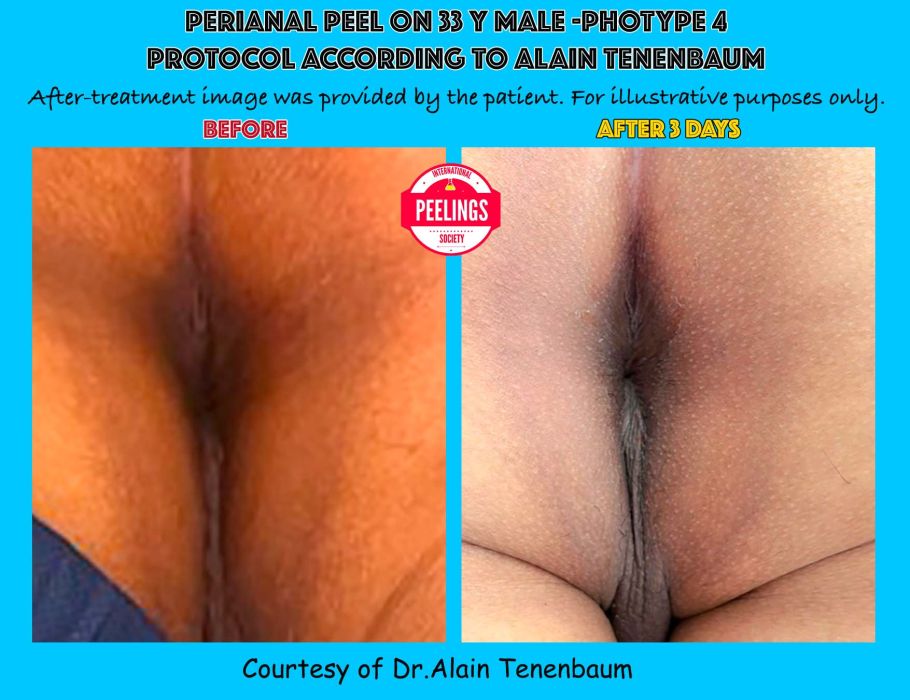
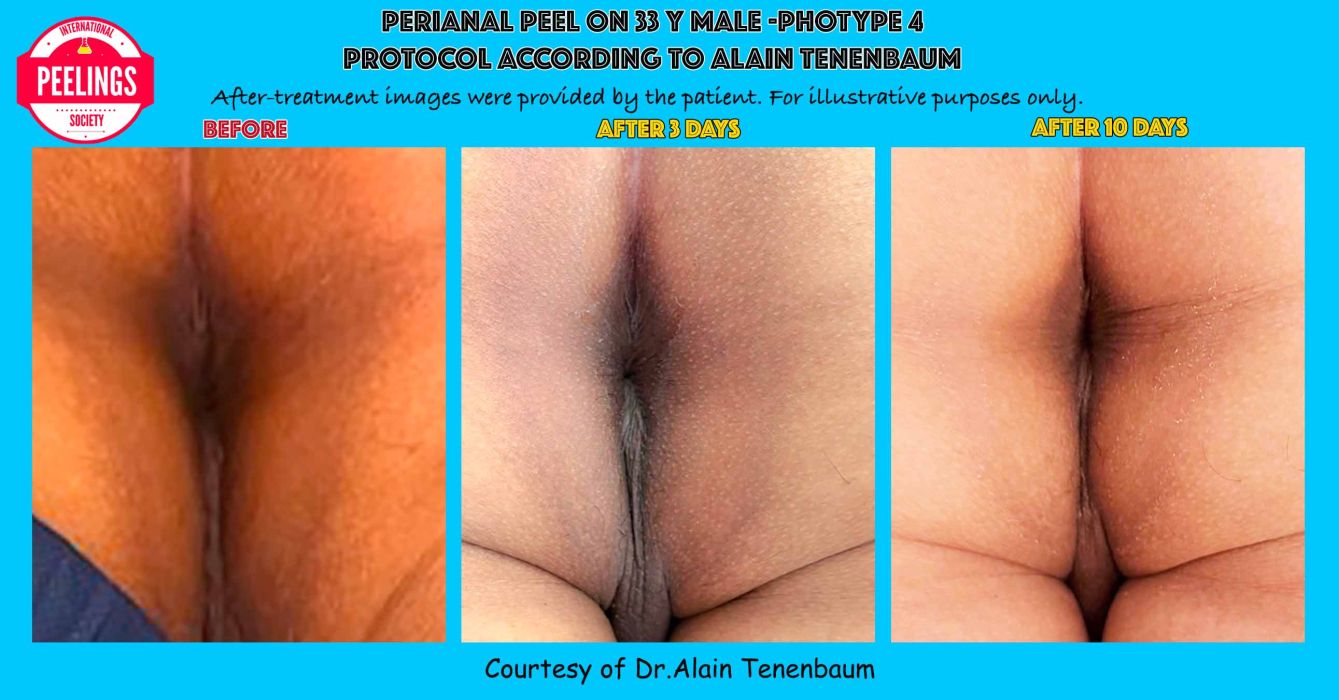
Please repeat each session, following all steps, once each 2- 3 weeks for 6 sessions ( average)
Ideally, the procedure should be scheduled at least three days before a period of sexual abstinence.

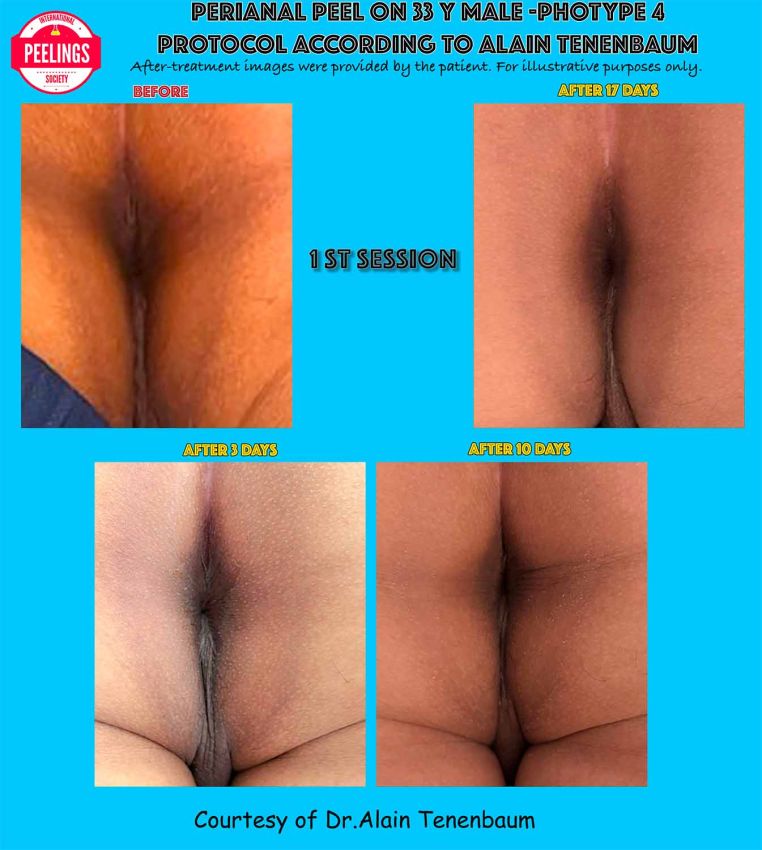
It is normal to experience sometimes a socially noticeable appearance for about three days following the initial session, known as the attack phase of the treatment. It is especially important not to panic during this period.
This temporary appearance often seems worse than before, particularly around the third day after both the first and second sessions. However, by the third day following the third session, any remaining discoloration (dyschromia) typically does not warrant social withdrawal. By the third day after the fourth session—the skin generally appears almost entirely free of visible discoloration.
It is crucial that the patient continues with the full course of treatment, regardless of temporary setbacks.
Interrupting the treatment or switching physicians mid-process can result in outcomes that are worse than the initial condition and may persist for a significantly longer period. At this stage, patient responsibility is key.
Additionally, it is essential that the patient refrains from using any personal cosmetic creams during the treatment period.
Lipoic Acid Cream offers significant benefits in clinical and aesthetic applications. Lipoic acid is known for its ability to enhance the transdermal penetration of active ingredients, facilitating their delivery into the deeper layers of the epidermis and dermis.
Recommended Combinations:
For deeper hyperpigmentation: Combine with StretchPeel (Depigmenting Cream) to optimize depigmenting effects beyond the superficial layers.
For dehydration of the deeper skin layers or in mature skin: Combine with Les Félins (Moisturizing Cream) to restore hydration and improve skin resilience.
This targeted approach allows for more effective and personalized treatment protocols based on individual skin conditions.
Stretchpeel is the ultimate depigmenting cream, thanks to its carefully selected ingredients and its alcohol-free formulation. It does not contain hydroquinone—a drug often associated with complications such as hypochromia.
As stated by Dr. Alain Tenenbaum and Mr. Mauro Tiziani, the goal is not to erase color variations, but to transform the mosaic of skin tones (hyperpigmentation) into a harmonious balance of intime areas complexion.
Les Félins Moisturizing Cream truly deserves its name, as it is designed to help prevent your dyschromia from turning into feline-like spots. This product has the advantage of being non-greasy and absorbing much faster than other moisturizing creams. It is alcohol-free and contains no ingredients that could cause complications.
You can apply this cream as often as you like, with no limitations.




To rehydrate the skin:
A peel removes part of the stratum corneum (the skin’s outermost layer), which temporarily reduces the skin’s ability to retain moisture. This leads to dryness and sensitivity. A moisturizer helps restore lost hydration.
To strengthen the skin barrier:
Hydrating ingredients help rebuild the skin’s protective lipid barrier, reducing irritation, redness, and tightness.
To minimize excessive flaking:
While some flaking is normal after a peel, moisturizing the skin helps reduce discomfort and makes the process more tolerable and discreet.
To support cellular regeneration:
Well-hydrated skin heals faster and supports more efficient cell turnover, optimizing the benefits of the peel.
Specially formulated:
Post-peel cream typically contains soothing and restorative ingredients (like panthenol). They are free from irritants such as alcohol, fragrance, or harsh preservatives.
To prevent complications:
Using appropriate post-peel care helps reduce the risk of irritation, inflammation, or post-inflammatory hyperpigmentation—especially important for sensitive or darker skin tones.
To enhance results:
Proper post-treatment care maintains and prolongs the benefits of the peel, including improved radiance, smoother skin texture, and a more even tone.
Daily sun protection (broad-spectrum like Stretchpeel) is essential for several weeks to months following a peel.
Avoid harsh products such as retinoids, acids, or exfoliants during the skin’s recovery phase.


Monitor pigmentation changes.
Evaluate if additional peels or other treatments are appropriate.
Avoid heat exposure (saunas, hot yoga).
Limit hormonal triggers (e.g., oral contraceptives, if relevant).
Treat underlying inflammation, which can worsen pigmentation.




Hyperpigmentation is a common skin concerns caused by excess melanin production, often triggered by sun exposure, hormones, or inflammation. The best way to manage these conditions is through consistent prevention. Here's how to protect your skin and reduce the risk of uneven tone:
Harsh or irritating products can worsen pigmentation and damage your skin barrier.
Cleanse Gently: Use a mild, non-stripping cleanser like Aseptiskin
Avoid Irritants: Stay away from products with alcohol, fragrance, or abrasive exfoliants. (more than 98.9% of cosmetics an sunscreens are damaging your skin)
Moisturize Daily: Keep your skin hydrated with Les Félins that support barrier health.
Intime Areas Hyperpigmentation is often linked to hormonal changes such as pregnancy, birth control use, or hormone therapy.
Talk to Your Healthcare Provider If you're noticing skin changes related to medications or hormones.
Certain ingredients can help regulate melanin production and prevent discoloration.
Niacinamide (Vitamin B3) – Helps reduce pigment transfer and inflammation.
Vitamin C – A powerful antioxidant that brightens and protects the skin.
Azelaic Acid – Calms inflammation and helps fade dark spots.
Tranexamic Acid –
Arbutin and Licorice Extract – Natural brighteners that support an even skin tone.
Don’t Pick at Skin: Picking, scratching, or over-exfoliating can lead to post-inflammatory hyperpigmentation.
Manage Stress: Chronic stress can affect hormone levels and skin health.
Eat a Balanced Diet: A diet rich in antioxidants supports overall skin resilience.
Tanning beds and prolonged sun exposure
Unsupervised use of strong medical treatments like hydroquinone or topical steroids

Add a barrier/protective agent:
Zinc oxide ointment
or Dexpanthenol ointment (rectal formulation if available).
Apply a topical greasy antibiotic ointment into such as:
Oxytetracycline ointment (if available for rectal use).
Alternative: gentamicin or fusidic acid ointment.
Add a barrier/protective agent:
Zinc oxide ointment
or Dexpanthenol ointment (rectal formulation if available).
Apply a topical greasy antibiotic ointment into such as:
Oxytetracycline ointment (if available for rectal use).
Alternative: gentamicin or fusidic acid ointment.

We use cookies and similar technologies to improve your experience on our website.